Alzheimer’s Dementia

Written by Dr Estrelita van Rensburg
Introduction – Alzheimer’s dementia
Alzheimer’s dementia is such an alarming topic for most of us, obviously feared by many as 'a-too-ghastly-to-contemplate-disease' that may strike any time as we get older. Is the fear justified? Definitely, without a doubt. Losing one’s mind is close to the top of most people’s scary list.
Today, 40 to 50 million people globally are affected by Alzheimer’s disease, with a projected increase of over 200 percent over the next 30 years.1 Moreover, this is truly a pandemic with most of us knowing someone who is already affected. The disease is progressive and most importantly, no medications developed thus far have a meaningful impact to stop it.
On top of that, the care for patients with Alzheimer’s disease is very costly, reaching $1 trillion globally and projected to double by 2030.2 It is a significant contributing factor in bankrupting our global healthcare systems and, on a more personal level, emotionally and financially damaging for families and carers of Alzheimer patients. However, if this was the whole story, I could stop writing this article right here. But is it?
NO, it is not. We definitely need to address the issues that are causing the rapid rise of this disease. What's more - there is hope for all of us in being able to prevent this devastating condition.
Alzheimer’s dementia is mostly preventable
Alzheimer’s disease is by and large a preventable disease. Surprisingly, only about five percent of cases are genetic (Familial Alzheimer's dementia). The vast majority is preventable simply by making personal healthy lifestyle choices that support brain health throughout our lifetime. Our brain is resilient and every little bit we do helps. Truly a message of hope to us all. The price we must pay, though, requires discipline and commitment.
Symptoms of the disease typically present later in life, although the disease process starts years to decades earlier. Unhealthy lifestyle choices can already cause changes in the brain of young people in their twenties. Most however, are completely unaware of this, since symptoms only manifest decades later.3 It is therefore never too early (or too late) to start implementing healthy habits, primarily because of our brain’s fantastic ability to regenerate itself through neurogenesis (the ability to create new brain cells throughout a person’s lifetime) and neuroplasticity (the ability to rewire and reshape its networks).
Neuroplasticity the ability to rewire and reshape neural networks
Even people carrying the APOE ε4 gene, generally associated with an increased risk for developing Alzheimer’s dementia, can offset this risk by appropriate lifestyle changes. The world of epigenetics shows that our genes are not our destiny, because genetic plasticity or the expression of genes can be influenced by many factors, e.g., the food we eat and environmental pollutants.
Alzheimer's disease is diabetes of the brain
In 2005, the physician-scientist and neuropathologist Dr. Suzanne de la Monte reported that Alzheimer’s disease was a form of diabetes and coined the term ‘Type 3 Diabetes’ or diabetes of the brain.3 Seen this way, type 2 diabetes is diabetes of the body. This discovery finally opened a whole new way of thinking for scientists investigating the disease.
In our body, the hormone insulin produced in our pancreas, is required to keep our cells working including the neurons in our brain, by regulating blood glucose levels. When blood glucose levels rise (after eating carbohydrate-rich food), insulin levels rise in order to lower glucose levels back to normal. High insulin levels over time lower the sensitivity of our cells to respond to the effects of insulin. This condition is called ‘insulin resistance’ and may take years, even decades, to develop.
Sugar, carbs, and man-made oils are damaging the brain
Carbohydrate-rich food (starch and sugar) is found in processed food and not to mention drink items that so many people binge on daily. They are available everywhere we go—stacked on supermarket shelves, in prominent display areas in corner shops, next to the payment booth at petrol-filling stations, fast-food outlets, and street vendors—penetrating the remotest corners of the globe.
The result of the modern fast-food/convenience diet is that insulin levels in the body are driven to increasingly higher levels over time. Eventually, while trying to cope with the sugar/glucose overload to which our body and brain are constantly exposed, the glucose metabolism system becomes dysfunctional, leading to cell death.
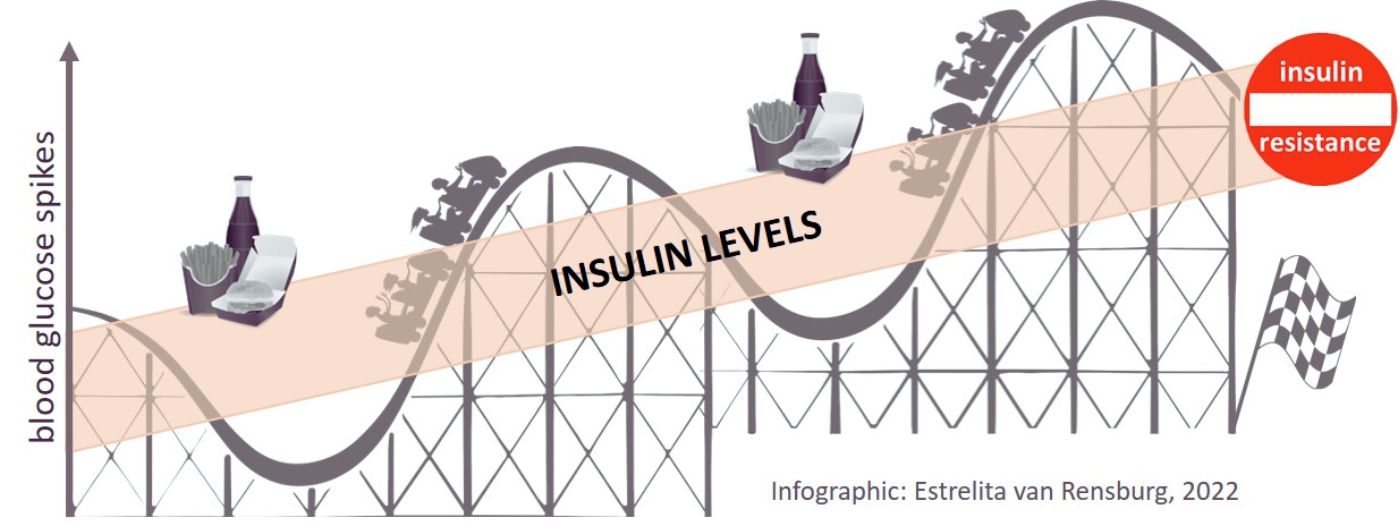
Insulin resistance develops over time when following a high carbohydrate diet
In Alzheimer’s disease, the brain becomes more sluggish as insulin resistance progresses since it impacts normal brain cell function. The cells of the brain's memory centre (hippocampus) are especially sensitive to these changes. They are the first neurons to be impacted by insulin resistance. As the disease progresses, other brain areas become affected as well, resulting not only in memory loss but a gradual decline in cognitive brain function. Eventually, the disease leads to death, typically occurring three to nine years after diagnosis.
Chronic inflammation of the brain is another very important aspect of Alzheimer’s disease. Sugar overload leads to fluctuations in brain glucose levels which drive the over-production of damaging free radicals (waste products from cellular reactions) in our brain cells. In addition to this, the consumption of industrially-produced vegetable/seed oils (made from corn-, sunflower-, safflower-, cottonseed-, and soybean seeds), increases levels of omega-6, a powerful pro-inflammatory molecule.5,6
Risk factors for developing Alzheimer’s disease
The commonly recognized risk factors:
- type 2 diabetes (doubles the risk)
- female (twice as likely to develop Alzheimer’s disease compared to men)
- overweight/obesity
- genetic markers
- age (>65 years)
Knowing these risk factors helps us to understand the disease’s root cause. The tragedy is that insulin resistance is rarely diagnosed in clinic or GP practices; hence patients are not warned that they have it, nor about the subsequent consequences such as heart disease, type 2 diabetes, certain cancers, and Alzheimer’s dementia. On the contrary, advice or treatment is usually given when one or more of these diseases are already present.
Prevention and treatment strategies for Alzheimer’s dementia
Drug treatment has no effect on the underlying condition of insulin resistance; drugs will not put it into remission nor prevent the development of one or more lifestyle diseases. The only effective treatment is to remove the root cause of insulin resistance, which is accomplished by changing our diet. We are not talking about a standard yo-yo calorie-restricted diet that still allows the consumption of carbohydrate-rich and industrialized-oil processed foods.
We can all do things every day that will keep our brains healthy. If the brain is already impacted, for instance by mild cognitive impairment (which is not necessarily synonymous with progression to Alzheimer’s disease), brain function can still be improved. Mainstream medicine is often resistant to the idea that the simple strategies listed below can have an effect, despite the fact that data out there shows that it is possible. The most important factors are:
- diet (as mentioned above, this is not the traditional calorie-restricted diet)
- exercise
- sleep
- keep stress levels down
- train your brain
Diet is the primary driving force
Diet is the primary force driving insulin resistance in the body. The rates of lifestyle diseases such as dementia, heart disease, diabetes, certain cancers, and obesity have risen dramatically since the introduction of dietary guidelines in the US in 1980 and a few years later in the UK.7 To improve or reverse insulin resistance, it is important to revert to a diet based on eating real whole foods. Avoid refined carbohydrates such as sugar, flour, rice, pasta, fruit juice, and processed cereals as much as you possibly can. Kick the habit of consuming energy bars, juice boxes, bagels, donuts, and other temptations to the side.
Follow a brain smart diet. Cook like your great-grandmother did—real food comes without labels! Eating real food, rich in natural protein and fat with a very limited amount of carbohydrates (starch and sugar), will result in decreasing insulin levels. This will help the body to start burning fat and generate ketones, a very healthy alternative energy source for the brain that is not dependent on insulin.8
Exercise and sleep
Exercise helps the brain in so many ways. It increases the insulin sensitivity of cells, promotes the growth of new brain cells, increases the supply of oxygen and nutrients to the brain, and removes toxic substances (detoxes the brain). It also helps improve our stress levels and should always be prioritized as a core component of a healthy lifestyle.
Impaired memory, reduced alertness, and mental health instability have all been associated with insufficient sleep. Humans need more than seven hours of sleep each night to maintain cognitive performance. Moreover, improving regular sleep quantity and quality are so important for new learning and memory embedding. It even has healing abilities for the minds of many people suffering from psychiatric conditions. Think of sleep as the cleansing process that removes toxic metabolic waste products and stress molecules from the brain. Memories formed without sleep are weak and evaporate rapidly. No wonder sleep disturbance often precedes the onset of Alzheimer’s dementia by several years.9

Sleep is important for brain health
Stress, our gut and brain plasticity
A body exposed to chronic stress is toxic for the brain. Stress changes the hormone equilibrium in our body. It increases cortisol levels, which in turn increase glucose levels, resulting in inflammation and the damaging effects of oxidative stress, especially in the sensitive memory storage area of the brain.
Another factor is the health of our gut microbiome, which impacts our brain performance. These body-friendly gut organisms produce important chemicals that interact with all the cells in our body, including our brain cells. This important two-way system that connects the gut and brain, is called the 'gut-brain axis.' Factors such as stress, antibiotics, glyphosate (a herbicide frequently contaminating plant-based foods), and wheat-based products (causing increased intestinal permeability or leaky gut) all harm our gut microbiome. An affected or sick microbiome produces peptides and enzymes that not only impact our immune system but also damage our brain cells (neurotoxins).10
Finally, the brain, like any other machine, needs to be regularly oiled. This is done by continuous activity and learning. Stimulate your brain, for instance, read, learn a new language, learn to play an instrument, etc. The possibilities are endless on how to increase your brain’s plasticity and prevent cognitive decline. We are never too old to learn new things!

Learning is important to keep stimulating the brain
Preventing Alzheimer's dementia is up to you
In conclusion, we now understand that even scary diseases over which we thought we had no control, can be prevented through following a healthy lifestyle, especially by changing our diet. It is not something we buy from the pharmacy. It is up to us to take responsibility for our own health. Help is available if you need guidance on how to implement these important dietary changes. Make it part of your own healthy lifestyle.
References
- Alzheimer’s Research UK, Dementia Statistics Hub, accessed August 2022.
- Prince, M et al. World Alzheimer Report 2015, The Global Impact of Dementia: An analysis of prevalence, incidence, cost and trends. Alzheimer’s Disease International, 2015.
- Castellano CA, Baillargeon JP, Nugent S, Tremblay S, Fortier M, Imbeault H, Duval J, Cunnane SC. Regional Brain Glucose Hypometabolism in Young Women with Polycystic Ovary Syndrome: Possible Link to Mild Insulin Resistance. PLoS One. 2015 Dec 9;10(12):e0144116
- de la Monte SM, Wands JR. Alzheimer's disease is type 3 diabetes-evidence reviewed. J Diabetes Sci Technol. 2008 Nov;2(6):1101-13.
- Watt C, Sanchez-Rangel E, Hwang JJ. Glycemic Variability and CNS Inflammation: Reviewing the Connection. Nutrients. 2020 Dec 21;12(12):3906.
- Simopoulos AP. The omega-6/omega-3 fatty acid ratio, genetic variation, and cardiovascular disease. Asia Pac J Clin Nutr. 2008;17 Suppl 1:131-4. PMID: 18296320; Teicholz N. The Big Fat Surprise. New York, NY: Simon and Schuster; 2014.
- US Department of Health and Human Services and Department of Agriculture. Nutrition and Your Health: Dietary Guidelines for Americans, Washington, DC: US Government Printing Office; 1980.; National Alzheimer’s diseasevisory Committee on Nutritional Education (NACNE). A discussion paper on proposals for nutritional guidelines for health education in Britain. London: The Health Education Council, 1983.
- Volek J., Phinney, SD., Kossoff E., Eberstein JA., & Moore J. The art and science of low carbohydrate living: an expert guide to making the life-saving benefits of carbohydrate restriction sustainable and enjoyable. Lexington, Beyond Obesity. 2011.
- Walker, M. Why We Sleep. Penguin Books, UK, 2017.
- Lukiw WJ. Gastrointestinal (GI) Tract Microbiome-Derived Neurotoxins-Potent Neuro-Inflammatory Signals from the GI Tract via the Systemic Circulation into the Brain. Front Cell Infect Microbiol. 2020 Feb 12;10:22.

